INTRODUCTION
A diagnosis of oesophageal cancer will be confronting for not just our patients, but their family, friends and workmates. The Royal North Shore Hospital prides itself on having some of the best medical staff in the country. Our team includes cancer surgeons, radiation oncologists and medical oncologists, radiologists, pathologists, nursing and allied health staff. Our care is focused on the patient and their family whilst striving to obtain the best possible outcomes. All our new cases are discussed in a special meeting of all our team (called a multidisciplinary meeting or “MDT”) to ensure everyone is involved in the patient’s care from the very beginning of their cancer journey.
Chemo-radiation is used either as pre-operative treatment prior to a planned operation or as sole treatment aimed at eradicating all cancer within the oesophagus and surrounding lymph glands. Your cancer doctors will outline your treatment pathway, the likelihood of success and any risks involved. The aim of this booklet is to outline what is involved with receiving chemo-radiation, possible side effects and what can be done to help.
The Department of Radiation Oncology at RNSH is equipped with the most advanced technology, enabling us to provide some of the highest quality radiation treatment in Australia dedicated to not only providing the best chance of cure but also to keep the risk of unwanted side effects to a minimum. Our Radiation Oncologist Associate Professor Andrew Kneebone has a specific treatment focus on oesophageal cancer, and his dedicated team continue to expand the Royal North Shore Service oesophageal cancer treatment service into the 21st century.
WHY RADIOTHERAPY AND WHAT IS INVOLVED?
 Radiotherapy is designed to destroy cancer cells in the designated treatment area, while at the same time, trying to limit damage to any surrounding normal cells.
Radiotherapy is designed to destroy cancer cells in the designated treatment area, while at the same time, trying to limit damage to any surrounding normal cells.
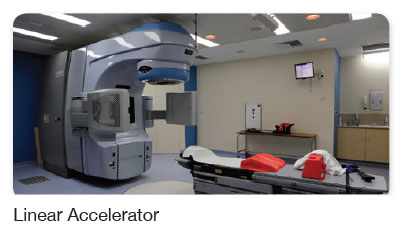
The cancer in the oesophagus is treated, as well as the areas surrounding the oesophagus, including the adjacent lymph glands where the cancer can possibly spread to. High energy x-ray beams are directed at the oesophagus from outside the body using a machine called a linear accelerator.
These beams damage the cancer cells and stop them from dividing and growing. The cancer cells are not able to recover from this damage and subsequently die. However, the normal healthy cells, which mostly have the ability to repair themselves, recover and survive.
Should you have any questions about the radiotherapy and the treatment field, your radiation oncologist will happily explain this information in more detail.
CLINICAL RESEARCH
Ongoing research into treating oesophageal cancer with a view to improving treatment outcomes for patients, is a key focus for the Department of Radiation Oncology at RNSH.
RNSH is affiliated with the University of Sydney and the Department of Radiation Oncology here at RNSH, prides itself in actively participating in research. As RNSH is a leading Australian site for the delivery of new radiation therapy technology, it is very important that data on all patients receiving treatment is collected. You will be asked if you agree to participate in this research and we would very much appreciate your support here.
RNSH is currently one of the only radiation oncology centres in Australasia affiliated with the United States Radiation Oncology trials group (RTOG). This allows the treatment team at RNSH, the potential to offer patients the latest in oesophageal cancer research.
RADIATION THERAPY PLANNING AND TREATMENT
Radiation treatment to the oesophagus generally involves 25 – 30 treatment visits (usually 28) to the radiotherapy department over a period of approximately 6 weeks. It generally takes between two and four weeks to organise your radiation treatment. Radiotherapy is a very precise treatment that is tailored for each patient as it is extremely important to be accurate with the delivery of this radiation. All patients are treated with “image guided radiotherapy”. This means that the treatment position is checked daily prior to treatment with special x-rays taken while on the treatment couch.
THE PLANNING SESSION (SIMULATION)
 At the planning appointment you will have a CT scan (simulation) of your chest and upper abdomen. The CT scan (simulation) is performed in the Department of Radiation Oncology. Three permanent skin tattoos are used as reference points to mark the area we plan to treat. They are the size of a small freckle and are given with a small needle into the skin. They will also use some temporary texta ink marks on your skin. These texta marks can be
At the planning appointment you will have a CT scan (simulation) of your chest and upper abdomen. The CT scan (simulation) is performed in the Department of Radiation Oncology. Three permanent skin tattoos are used as reference points to mark the area we plan to treat. They are the size of a small freckle and are given with a small needle into the skin. They will also use some temporary texta ink marks on your skin. These texta marks can be
washed away after the planning session.
 For the planning visit, please bring any past CT scans or other xrays on the day. In most cases, you will have had a PET scan performed prior to the radiotherapy planning session. If this was performed at RNSH, this will be transferred automatically to the planning computer which will allow the radiation oncologist to accurately idenify the area that needs treatment. If your scan was done at another centre, please tell your radiation oncologist and arrangements will be made for the disc of the PET scan to be transferred across.
For the planning visit, please bring any past CT scans or other xrays on the day. In most cases, you will have had a PET scan performed prior to the radiotherapy planning session. If this was performed at RNSH, this will be transferred automatically to the planning computer which will allow the radiation oncologist to accurately idenify the area that needs treatment. If your scan was done at another centre, please tell your radiation oncologist and arrangements will be made for the disc of the PET scan to be transferred across.
You will also see the dietician to advise you on maintaining a healthy diet and how to reduce some of the side-effects of treatment by modifying your diet. The dietician will monitor you closely during your time of treatment.
YOUR TREATMENT SCHEDULE
The radiation therapists will provide you with your schedule of treatment appointments at the Planning Session. This will include the time and date when you will be starting your treatment. It is important that you discuss any concerns with your treatment schedule with the Radiation Therapist at this time.
You will be able to drive yourself to the department for treatment and continue with your usual daily activities, such as working.
UNDERGOING RADIATION THERAPY TREATMENT
The radiation therapists (RTs) give the actual radiation therapy treatment. Each treatment session takes about 15 minutes, however, you are likely to be at the Cancer Therapy Centre anywhere between 30 and 60 minutes (depending upon the number of patients waiting and if the machines are on schedule).
- When you arrive, you first need to check in at our Reception.
- Proceed to the waiting room. From here, radiation therapy staff will call your name and ask you to change into a hospital gown. After this, you will then be asked to wait in the waiting area next to your treatment machine.
- When the RTs are ready for you, they will call you into the treatment room, where you will be asked to lie on the treatment couch. Most of the time in the room will be spent making sure that you are in the correct position and checking that the same area receives radiation on each visit. x-rays are taken on a regular basis to ensure you are in the correct position for treatment.
TREATMENT DAYS & OTHER APPOINTMENTS
Radiation therapy treatment is given daily, on weekdays only. There is no treatment offered on weekends or public holidays. However, we try to ensure that patients are treated 5 times each week which in some cases may lead to you being treated twice in the one day (6 hours apart) to make up for missing a day because of a public holiday or another reason. The machine staff will inform you of any changes needed to your treatment schedule.
You will also be asked to attend the radiation therapy clinic every week, so that you can be reviewed by your specialist or their registrar (a Radiation Oncology specialist-in-training). They will also discuss with you, any side effects or concerns you may have with treatment. The radiation oncology nurses will also organise for you to have a blood test each week to ensure your body is handling the radiation and chemotherapy treatment well.
SIDE EFFECTS OF RADIOTHERAPY
Side effects vary markedly from person to person. Some people can handle treatment very well and can maintain their work commitments. Other people can have a very difficult time and may need to come in to hospital so their side effects can be looked after.
The chemotherapy weeks (usually the first and fifth weeks) can be difficult for some patients and sometimes your medical oncologist will arrange for you to be kept in hospital during this time. Maintaining an adequate diet throughout treatment is the key to minimising side effects and the team will work hard to ensure you maintain your weight during treatment.
Many working people find that they can still attend work through-out the non chemotherapy treatment period of the radiation, usually with some adjustment of their work hours. However, towards the end of radiotherapy the majority will need to take significant time off work (often the last 2 weeks of chemo-radiation and the two weeks following). Please discuss with your cancer doctors the potential impact of treatment on your ability to perform your work duties.
EARLY REACTIONS – (i) COMMON
Tiredness
This is a common side effect although the amount of tiredness varies from person to person. Most people find that they can still perform many of their normal daily activities but will find they tire more easily (especially towards the end of treatment) and many require an afternoon rest.
Sore oesophagus
It is usual to develop some heartburn type symptoms by about the third week of treatment. You may have difficulty and some discomfort when you eat meals. This will usually persist until about 3 – 4 weeks after the radiotherapy has finished. During this time you may need to change your diet to soft or pureed foods. We have a dietician available to discuss your diet during treatment and to supervise what you eat. Just ask a member of staff to help you.
It is usually helpful if you avoid certain foods and drinks that irritate the oesophagus such as acidic fluids (such as fruit juices), hot curries, coffee and tea and foods or drinks that are very hot or very cold. In some situations the sore oesophagus gets so severe that you may be prescribed some strong pain killers. In about 20% of cases you may need to be admitted into hospital for either fluid via a drip or through a small feeding tube placed in your stomach. Your doctor can discuss this with you if that is worrying you.
Skin reddening and irritation
Slight skin reddening and dryness of the skin on the chest and back can occur by the 2nd to the 3rd week of treatment. The skin becomes redder towards the end of treatment. This reaction settles usually over 2 – 4 weeks after the completion of therapy. Irritation is generally relived by Sorbolene Cream. If the reaction worsens, your doctor may prescribe a cream for you.
Temporary loss of hair
Temporary loss of hair may occur on your chest and back. The hair on your head will not be affected.
EARLY REACTIONS – (ii) UNCOMMON
Nausea
 Nausea from the radiation is relatively uncommon though may occur
Nausea from the radiation is relatively uncommon though may occur
during the chemotherapy week. If it does occur, medication can be given
to relieve this. Speak to your doctor if this occurs.
Please mention any problems to the radiation therapists or radiation nurses
giving you your treatment. Your doctor will also see you regularly during
treatment so problems can be discussed at these visits.
LONG TERM EFFECTS
The majority of patients make a good recovery from their radiation treatment and do not experience side effects that are a bother to them, in the long term. Occasionally, however, some patients may experience some side effects that may persist, or even start, many months after the radiation treatment has finished.
Common
There are really no common long-term effects of the treatment. In about 20% of cases some patients will develop some scarring in the oesophagus that makes the oesophagus narrow (called a stricture). Sometimes this needs to be fixed by a small procedure. We can discuss with you further if it is necessary.
Uncommon
The radiation has to travel through some lung tissue before it hits the tumour. When planning your radiation we try to keep the amount of lung treated to a minimum. However, there is a small risk that the lung can be damaged by the radiation, resulting in either temporary or permanent shortness of breath. This is particularly the case if you have previously been a heavy smoker or continue to smoke. We recommend that you cease smoking during and after the radiation. Your doctor can discuss the risk to your lungs in your particular case. In general, the risk for permanent damage is about 5%. It is important that if you develop shortness of breath or cough 2 – 12 months after radiation that you request consultation back with the radiation oncologist who looks after you.
Extremely Rare
Unusual, extremely rare complications can occur with any treatment including surgery or radiation therapy. Radiation has been known to cause a rare tumour (sarcoma) in about 1 in 1000 cases. Also extremely rarely the spinal cord can be damaged by radiation resulting in paralysis. The chances of this occurring are estimated to be <1 in 1000 cases.
