WHAT IS AN OESOPHAGECTOMY?
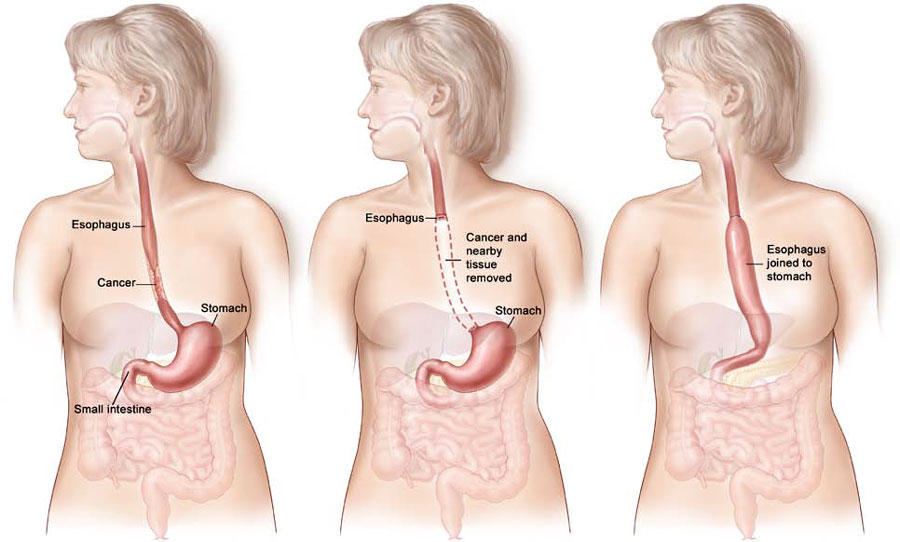
An oesophagectomy is the removal of most of the oesophagus. The main function of the oesophagus is to transport food from your mouth to your stomach. When a section is removed the two ends are joined back together (anastomosed) which means the stomach is higher up then before. In fact the stomach after the operation will be situated more inside your chest than your abdomen but will function almost normally in this position. The amount of oesophagus that is removed will depend on the size and position of the cancer.
Types of OESOPHAGECTOMY
IVOR LEWIS OESOPHAGECTOMY
This surgery involves an incision in the abdomen (laparotomy) and then an incision in the right side of the chest between the ribs (thoracotomy).
THORACOSCOPIC ASSISTED OESOPHAGECTOMY
This type involves an incision in the abdomen (laparotomy), keyhole incisions in the right side of the chest (thoracoscopy) and an incision in the left side of the neck.
RADICAL’ OESOPHAGECTOMY
The term “radical” describes the removal of lymph glands around the stomach and oesophagus. Surgery for oesophageal cancer and pre-cancerous lesions generally involves a radical oesophagectomy.
The type of oesophagectomy performed on an individual patient will be determined principally on the position of the tumour or disease.
An oesophagectomy is a very large operation and may take from between five and ten hours to perform. The anaesthetic and surgery is complex and require a specialist anaesthetist and a team of surgeons to perform.
The aim of the surgery is to remove the tumour with a clear margin.
All removed tissue including any lymph nodes are sent for pathological assessment. Results of these tests are normally back within 5 – 7days.
POSSIBLE RISKS & COMPLICATIONS
- Wound infection
- Chest infection/Pleural effusion
- Anastomotic leakage at the site where the digestive system was reattached.
- Deep Vein Thrombosis (DVT)
- Haemorrhage
- Abscess
The risk of dying from this procedure is very low, 1 – 3%. However the risk of a minor complication is approximately 40%. You will be carefully monitored by your surgeon and nursing staff to prevent these complications.
Also taking the IMPACT supplement drinks for five days prior to your surgery has shown to promote wound healing and reduce the risk of complications. Either the dietician or Cancer Nurse Coordinator will speak with you about the benefits of these supplements and they can be purchased through your specialist rooms at a discounted price.
YOUR STAY IN HOSPITAL
 Your operation will be performed in either Royal North Shore Hospital or North Shore Private Hospital. Prior to surgery you will need to attend the pre admission clinic this takes generally a few hours. At this appointment you will see an anaesthetist, have bloods taken, and then be assessed by the nursing staff and a physiotherapist. You will be given a contact phone number to call on the day prior to surgery to find out the time you will need to come into hospital on the following day and when to fast from. Your surgeon will contact your relatives to tell them how the operation went and to discuss the findings.
Your operation will be performed in either Royal North Shore Hospital or North Shore Private Hospital. Prior to surgery you will need to attend the pre admission clinic this takes generally a few hours. At this appointment you will see an anaesthetist, have bloods taken, and then be assessed by the nursing staff and a physiotherapist. You will be given a contact phone number to call on the day prior to surgery to find out the time you will need to come into hospital on the following day and when to fast from. Your surgeon will contact your relatives to tell them how the operation went and to discuss the findings.
You will stay approximately 14 days after your surgery. You will spend between one and three days in the intensive care unit. The breathing tube may also be left in for a few hours post operatively, but you should not be concerned because you will be drowsy that night and therefore will not remember much, including visitors.
For the first week you will have various intravenous drips which are used for hydration, a nasogastric tube to keep your stomach empty and a feeding tube. Your pain will be managed by an epidural, which will stay in place for about five days. These will all be removed as you progress through your recovery. You will also have chest drains which will be removed once your surgeon is happy with your recovery.
You will remain fasted for one week following the oesophagectomy. The feeding tube enters directly into the intestines, this gives the anastomosis the opportunity to begin healing prior to the introduction of food.
After one week, you will be given some blue dye to drink as well as some contrast to drink while being x-rayed. Both of these tests enable your surgeon to establish whether the anastomosis is healing adequately. If it is, then you will be offered some fluids to drink. If there is a delay in the healing of the anastomosis then the introduction of food and drink will be delayed.
You will be seen by the physiotherapist on a daily basis, and you will be encouraged to perform deep breathing and coughing exercises as well as mobilising. This is the most important thing you can do to help speed up your recovery and prevent pneumonia from developing.
The incision site will have numerous small metal clips that help keep the skin together. These will be removed before you leave hospital. This will not hurt you in anyway.
In some instances such as if you alone or having a slower recover it may be possible for you go to a local rehabilitation hospital for further care, or to have services to come into your home to assist you. You will not be discharged home until your surgeon is happy with your recovery progress.
AT HOME AFTER YOUR OESOPHAGECTOMY
 You have had a major operation and it will take 6-12 months to fully get back to how you were when you were well. Normally people feel quite well for the first couple of days at home and can over do activities. You may then find that on the subsequent days you will be lethargic and unmotivated, so it is important to take each day as it comes and listen to your body. If it needs a sleep, then do so.
You have had a major operation and it will take 6-12 months to fully get back to how you were when you were well. Normally people feel quite well for the first couple of days at home and can over do activities. You may then find that on the subsequent days you will be lethargic and unmotivated, so it is important to take each day as it comes and listen to your body. If it needs a sleep, then do so.
THINGS TO DO
We recommend to follow the dietary literature and advice given to you by the dietician while in hospital. If at any stage you have any dietary concerns or questions we can refer you to our dietician. You can engage in light physical activities including walking.
Intermittenty you will feel a sharp pain in the wound – this is just the muscles healing and you should not be concerned. As the weeks pass you will find yourself able to tolerate more activity and exercise.
WHAT TO AVOID:
Avoid heavy lifting for 3 – 4 weeks and you certainly should not drive for at least 3 – 4 weeks after your discharge.
CANCER NURSE COORDINATOR (CNC)
The Cancer Nurse Coordinator will contact you by phone regularly once you are discharged from hospital. You and your family can contact the CNC for advice, resources and support and because the CNC works closely with your surgeons she will keep them up to date of your progress.
The CNC when she contacts you will assess how your recovery from surgery is going and will include such questions about your diet, pain, wounds, bowels and mental wellbeing. From these assessments the CNC may feel that referrals to a dietician, physiotherapist, community nurses etc, may be necessary to aid your recovery process.
Contact with the CNC will allow you and your family to feel well supported and have an easy transition from hospital to home.
SURGEON CONSULTATION
 You will see your surgeon in his rooms 2 – 3 weeks after the operation and on this consultation you will probably have your feeding tube removed if it has not been done so already. Your surgeon will then advise you as to how regularly he would like to see you. You will be closely monitored with regular clinical reviews, CT scans and endoscopies.
You will see your surgeon in his rooms 2 – 3 weeks after the operation and on this consultation you will probably have your feeding tube removed if it has not been done so already. Your surgeon will then advise you as to how regularly he would like to see you. You will be closely monitored with regular clinical reviews, CT scans and endoscopies.